SURGERY RESEARCH INSIGHT
Summer 2023
East Carolina FireArm Injury Research
FAIR Alliance

Meeting with Sheriff Paula Dance – Pictured left to right: William Irish PhD, Chief Deputy Chauncey Congleton, Sheriff Paula Dance, Eric Toschlog MD., Reba Bullard
The recently created FAIR Alliance, a coalition of stakeholders in North Carolina formed under the direction of Dr. Eric Toschlog and the Divisions of Trauma and Acute Care and Surgical Research, is committed to supporting research and the evaluation of evidence-based practices to prevent firearm-related injury.
The Group’s objective is to collaboratively and proactively address firearm injury prevention in North Carolina through rigorous research and evidence-based practices. By fostering interdisciplinary partnerships and transdisciplinary approaches, we aim to advance knowledge and understanding in this critical area, seeking data driven and innovative solutions to mitigate firearm-related injury both intentional and unintentional ranging from primary prevention to public policy. This team recognizes that firearm violence is an intricate public health crisis in which we aim to utilize a unique complex system science analysis of firearm injury data to understand how these social determinants of health and co-morbidities affect firearm violence.
The FAIR Alliance Group is committed to establishing firearm injury prevention as a paramount priority in North Carolina, promoting the implementation of effective strategies, and supporting the next generation of researchers and practitioners dedicated to this cause. We strive to create a safer environment for our communities by increasing awareness, engaging with the public, and driving policy advancements based on our research findings and evidence-driven practices.
Within the first two months, the group has produced a submitted abstract entitled Gun Laws Matter: The Impact of Varying Legislation on Unintentional Firearm Hospitalizations, submitted to the 2023 National Research Conference for the Prevention of Firearm-Related Harms, November 1-3, 2023 in Chicago, IL, organized by the Research Society for the Prevention of Firearm-Related Harms.
Also, to note the significance of the moment on this specific topic, the most recent The North Carolina Medical Journal, featured firearm injury and violence prevention.
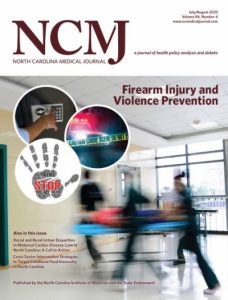
As a part of this feature, ECU trauma surgeon Dr. Eric A.Toschlog speaks with injury prevention epidemiologist Stephen W. Marshall about the role of clinicians and policymakers in deterring firearm injury and death in North Carolina and nationwide.
From January to September 2022, there were 2590 firearm-related emergency department (ED) visits in North Carolina,1 with the northeastern part of the state experiencing the highest firearm-related ED visits over the previous 12 months.2 Seeing what a firearm can do to the body has made Toschlog an advocate for consensus-driven, evidence-based policy to prevent firearm injuries and deaths in North Carolina and beyond.
In an interview with co-guest editor Stephen W. Marshall, director of UNC’s Injury Prevention Research Center, Toschlog argues for a shift in perspective among clinicians, policymakers, and firearm owners to view the gun injury and death crisis in a similar way to the opioid crisis.
Marshall S. “We Can Make Ownership Safer” – A Conversation with ECU Trauma Surgeon Eric Toschlog About Preventing Firearm Injury and Death. North Carolina Medical Journal. 2023;84(4). doi:10.18043/001c.81271
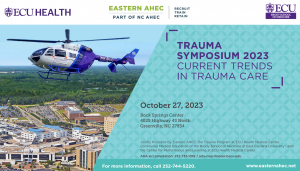
At the upcoming ECU Health Trauma Symposium 2023 this issue will again be front and center as our Guest Faculty Speaker, Dr. Brendan T. Campbell, will be discussing Firearm Injury: From Primary Prevention to Public Policy. Dr. Campbell has spoken at multiple institutions across the country and nationally including CNN.
2023 marks the 20th year of this annual symposium. Trauma clinicians will be able to update their knowledge of current evidence-based practices related to a wide variety of commonly occurring emergency conditions and responses. This symposium will address the identification, management and resuscitation strategies to manage adult and pediatric trauma in rural eastern North Carolina.
The program will conclude with an interactive panel of experts discussing special cases and responding to questions from the audience.
| Conference | Abstract Deadline |
|---|---|
| American Society of Clinical Oncology (ASCO) | 2/6/2024 |
| American Association for the Surgery of Trauma (AAST)(TACS) | 2/15/2024 |
| Military Health System Research Symposium | 2/21/2024 |
| American Public Health Association | 3/29/2024 |
| Resident and Fellow Trauma Paper Competition | The competition is open to all general surgery residents, surgical specialty residents, and trauma fellows. Medical students are not eligible. To be eligible for presentation at the COT Annual Meeting (Central competition), abstracts submitted may have been previously presented but not published as full papers in any peer-reviewed journal before March 30, 2024. |
| Obesity Week 2024 | 4/8/2024 |
| American Academy of Pediatrics (AAP) | 4/12/2024 |
| Conference | Conference Dates | Location | |||||
|---|---|---|---|---|---|---|---|
| Society of Thoracic Surgeons (STS) | 1/27/2024 | San Antonio, TX | |||||
| Southeastern Surgical Congress (SESC) | 2/3/2024 | Clearwater Beach, FL | |||||
| Association for Academic Surgery (AAS) | 2/6/2024 | Washington, DC | |||||
| Academic Surgical Congress (ASC) | 2/6/2024 | Washington, DC | |||||
| American College of Gastroenterology (ACG) | 3/8/2024 | Naples. FL | |||||
| Society for Clinical Vascular Surgery (SCVS) | 3/16/2024 | Scottsdale, AZ | |||||
| Society of Surgical Oncology (SSO) | 3/20/2024 | Atlanta, GA | |||||
| American Hepato-Pancreato-Biliary Association (AHPBA) | 4/4/2024 | Miami, FL | |||||
| American Society for Breast Surgeons | 4/10/2024 | Orlando, FL | |||||
| Society of American Gastrointestinal & Endoscopic Surgeons (SAGES) | 4/17/2024 | Cleveland, OH | |||||
| Association for Surgical Education (ASE) | 4/23/2024 | Orlando, FL | |||||
| American Urological Association (AUA) | 5/3/2024 | San Antonio, TX | |||||
| American Pediatric Surgical Association (APSA) | 5/16/2024 | Phoenix, AZ | |||||
| Plastic Surgery Research Council (PSRC) | 5/16/2024 | Boston, MA | |||||
| American Association of Plastic Surgeons (AAPS) | 5/18/2024 | Phoenix, AZ | |||||
| Digestive Disease Week/ Society for Surgery of the Alimentary Tract (SSAT) | 5/18/2024 | Washington, DC | |||||
| American Society of Clinical Oncology (ASCO) | 5/31/2024 | Chicago, IL | |||||
| American Society of Colon & Rectal Surgeons (ASCRS) | 6/1/2024 | Baltimore, MD | |||||
| American Transplant Congress (ATC) ASTS and AST joint meeting | 6/1/2024 | Philadelphia, PA | |||||
| Surgical Infection Society (SIS) | 6/5/2024 | Miami, FL | |||||
| American Society for Metabolic and Bariatric Surgery (ASMBS) | 6/9/2024 | San Diego, CA | |||||
| Society for Vascular Surgery (SVS) | 6/19/2024 | Chicago, IL | |||||
| Society of Black Academic Surgeons (SBAS) | 9/19/2024 | Sacramento, CA | |||||
| American College of Surgeons (ACS) | 10/20/2024 | Boston, MA | |||||
| American Thyroid Association ( ATA) | 10/30/2024 | Chicago, IL | |||||
| Southern Surgical Association (SSA) | 12/8/2024 | Palm Beach, FL | |||||
| San Antonio Breast Cancer Symposium | 12/10/2024 | San Antonio, TX |
First PCORI Submitted for Division of Surgical Research
“Research Done Differently”
Based upon a merit review process, our inter-departmental collaboration with the Department of Surgery and the Department of Health Services Information Management, Drs. Irish, Wong, and Burch were invited to apply to the PCORI Engagement Award Cycle 1. The primary long-term goal of this project is to improve treatment access for individuals with early-stage cancer that is potentially curative with surgery by (1) fostering collaboration between academic researchers and healthcare stakeholders to support the patient community in contributing innovative approaches to future patient-centered outcomes research and clinical comparative effectiveness research (PCOR/CER), (2) increasing the understanding of the importance of the patient community engagement to ensure research goals and dissemination of PCOR/CERresults are prioritized to those that are important to patients, and (3)enabling stakeholders to collaborate with researchers to incorporate their knowledge and experience directly in the design, implementation, and analysis of PCOR/CER.
Research funded by PCORI concentrates on healthcare challenges that confront families every day, including cancer, diabetes, maternal mortality, opioid addiction, mental health, and equitable access to care, among many others. Patients deserve to know whether some approaches work better than others for certain populations, and caregivers, clinicians, and all stakeholders also benefit from better information about different care options. With health, information is power and PCORI funds research that allows all patients to become more empowered decision-makers. Since its authorization by Congress in 2010, PCORI has awarded more than $3 billion to fund nearly 2,000 research and related projects.
PCORI’s holistic approach to generating and promoting the use of patient-centered evidence. There are four essential elements to this approach:
- Funding of patient-centered CER—to address questions important to patients and other stakeholders and to generate meaningful evidence that will allow them to make better informed health and healthcare decisions.
- Engagement—involving patients and all key health decision makers across the continuum of PCORI’s work, from research topic selection to dissemination and implementation of results, to produce research findings that are useful, relevant, and trustworthy to those we serve.
- Dissemination and Implementation—to ensure that the results of PCORI-funded studies are easily accessible and can be used by those who need them to make better informed decisions on health and healthcare.
- Research Infrastructure—including enhancing the ability of PCORnet®to improve capacity to conduct clinical research more efficiently, improving the science and methods of CER, and supporting the continuing development of the health research workforce.
Three Abstracts Accepted at ATC 2023

Dr. David Leeser attended American Transplant Congress, June 3-7 in San Diego, CA, representing the three East Carolina University co-authored abstracts accepted.
Clinical Utility of TruGraf Gene Expression Profile and TRAC dd-cfDNA in Immunosuppressant Adjustments: An Interim Report of the TRULO Study
C. Kew1, J. Fleming2, A. Frank2, A. Kawano2, J. Hickey2, L. Stach2, J. Weems2, J. Holman2, I. Agboli2, W. Irish3, S. Bunnapradist4, 1Univ of Alabama @Birmingham, Birmingham, AL,2Transplant Genomics, Inc, Framingham, MA,3East Carolina University, Raleigh, NC,4David Geffen School of Medicine, Los Angeles, CA
Impact of OmniGraf Results on Renal Function Changes Over a Year : An Interim Report of the Trulo Study
N. Leca1, C. Kew2, S. Westphal3, M. Karim4, S. Bunnapradist5, D. Leeser6, T. Alhamad7, J. Von Visger8, J. Fleming9, J. Holman9, J. Weems9, I. Agboli9, W. Irish10, F. Shihab11, 1University of Washington, Seattle, WA,2Univ of Alabama @Birmingham, Birmingham, AL,3University of Nebraska Medical Center, Omaha, NE,4University of Rochester Medical Center, Rochester, NY,5David Geffen School of Medicine, Los Angeles, CA,6East Carolina Univ Sch of Med, Greenville, NC,7Washington University School of Medicine at St. Louis, Saint Louis, MO,8Erie County Medical Center, Buffalo, NY,9Transplant Genomics, Inc, Framingham, MA,10East Carolina University, Raleigh, NC,11University of Utah Sch of Med, Salt Lake City, UT
Lack of Concordance Between TruGraf Gene Expression Profile and TRAC dd-cfDNA Results: An Interim Report of the TRULO Study
D. B. Leeser1, J. Fleming2, A. Frank2, J. Hickey2, A. Kawano2, D. Lazear2, J. Holman2, J. Weems2, I. Agboli2, W. Irish3, T. Alhamad4, 1East Carolina Univ Sch of Med, Greenville, NC,2Transplant Genomics, Inc, Framingham, MA,3East Carolina University, Raleigh, NC,4Washington University School of Medicine at St. Louis, Saint Louis, MO
Division of Surgical Research Attended
WCG MAGI East Clinical Research Conference
Sunday, May 21 – Wednesday, May 24, 2023
 In May 2023, three team members of the Division of Surgical Research attended the MAGI East Clinical Research Conference in Philadelphia, PA.
In May 2023, three team members of the Division of Surgical Research attended the MAGI East Clinical Research Conference in Philadelphia, PA.
To summarize, the WCG MAGI Clinical Research Conference is a unique 3.5-day event that connects more than 700 clinical research professionals who share a deep commitment to ensuring the quality, compliance, and efficiency of clinical research that is needed to advance the delivery of therapies and devices that impact patients’ lives. Attendees include representatives from sites, pharma, biotech, CROs, academia, government, regulators, and vendors. Conferences are twice a year to discuss best practices for clinical operations, business, and regulatory compliance, advance innovation, and network.
The comprehensive educational program offers varied learning formats including, panel discussions, lectures, topical solution roundtables, the WCG MAGI Innovation Theater, and pre-conference workshops focused on innovative solutions for day-to-day problems, best practices, career development, and current hot topics.
Attendees also have the opportunity to earn continuing education contact hours. Click here for more information.
-
Presence at ASMBS, Las Vegas on June 25 – 29, 2023

Members of the Division of Surgical Reseach and Department of Surgery gave two talks and two poster presentations in Las Vegas on June 25 – 29, 2023 at The American Society for Metabolic and Bariatric Surgery, the largest society in the world for the fields of metabolic and bariatric surgery.
POSTERS
Understanding Disparities in Access to Bariatric Surgery
Wong JH, Pories WJ. Burch AE, Irish WD
Bariatric surgery is the most effective treatment for sustained weight loss, and resolution of diabetes and other co-morbid conditions. Even so, utilization rates of bariatric surgery are low, especially in certain segments of the obese population. We sought to understand how health behaviors, clinical care, social and economic environment, as well as physical environment, contribute to disparities in access. Utilizing Wake as the reference county due to its ranking the highest in terms of health outcomes, we developed the Surgical Equity Index (SEI) as a measure to compare the observed vs the expected outcomes, that ranged from 0.15 to 0.95 (mean 0.47, SD 0.17) and was statistically significantly different in the 89 counties. Utilizing a hierarchical multivariable modeling approach, our results suggest that rurality is the most powerful predictor of disparities in access to bariatric surgery in North Carolina.
Fasting Lactate: A Marker for Early Metabolic Syndrome
Pories, WJ, Broskey, N, Jones, T, DeMaria, E, Ali, A, Houmard, J, Dohm, GL
Elevated lactate levels, indicators of mitochondrial inefficiency in the processing of glucose, are widely used in acute care as indicatof severity of injury and predictors of high mortality rates. Because lactate levels are also increased in the metabolic syndrome, we explored the concept that these might serve as early markers and as an approach to staging the syndrome.
We studied 57 healthy, athletic students, (24m/33f; BMI 27.0±2.31 kb/m2) enrolled in programs for training coaches. Fasting plasma lactate was 0.9 ± 0.3 mmol/L. Lactate was positively associated with visceral adiposity, triglycerides, HDL, HOMA-IR and systolic blood pressure, suggesting that lactate may be a biomarker for early metabolic syndrome.
TALKS
Effect of Bariatric Surgery on the Chronic Effects of Traumatic Brain Injuries
DeMaria, E
Patients with traumatic brain injuries frequently progress to obesity, T2D and the other expressions of the metabolic syndrome. Multiple reports, including our three-part review of the literature document that bariatric surgery improves mentation, brain function reflected by changes in functional MRI examinations and an increase in the volume of gray matter. The potential explanations include improved mitochondrial processing of glucose, the main fuel of the brain, improved mobility due to the loss of weight, correction of sleep apnea and, with the remission of the metabolic syndrome, a reduction in medications. Dr. DeMaria discussed the need for a prospective controlled study and our initial steps to develop such a trial.
Metabolic Surgery and Its Effects on the Metabolic Syndrome
Pories, WJ
The reasoning behind the broad effects of metabolic surgery with a reduction in severe obesity and T2D have yet to be explained.
Based on a review of the literature, as well as our studies in human subjects and cultures of striated muscle, the presentation proposed a hypothesis that the metabolic syndrome is due to dysmetabolic signaling from the foregut. Primarily identified from the gastric fundus, that interferes with the processing of glucose and fatty acids by mitochondria and metabolic surgery. By removing or bypassing the fundus, there was a reduction in most of the signal. Identification of the signal and the pursuit of evidence are urgently needed to combat the obesity and T2D epidemics.
Dr. Honaker Establishes a Research International Collaboration

Dr. Drew Honaker joins with international collaborators on several multi-institutional studies involving colon cancer.
- Dr. Drew Honaker- Department of Surgery, East Carolina University, Greenville, NC.
- Dr. Anas Taha and Dr. Vincent Ochs – Department of Biomedical Engineering, Faculty of Medicine, University of Basel, Allschwill, Switzerland.
- Dr. Anas Taha – Department of Surgery, GZO Hospital, Wetzikon, Switzerland.
- Dr. Stephanie Taha-Mehlitz – Clarunis, University Centre for Gastrointestinal and Liver Diseases, St. Clara Hospital and University Hospital Basel, Basel, Switzerland.
Dr. Honaker describes the various current collaborations with the group:
Dr. Taha initially reached out to the institution to collaborate on a multi-institutional, international project looking at patients that undergo bowel resection and associated mental health disorders. The goal of this study is to examine the impact of psychiatric and psychosomatic disorders, focusing on the patients undergoing small and large bowel surgery; as well as explore predictive modeling techniques to assess risk factors for higher morbidity.
As of today, among all institutions, there are over 7,000 patients entered into the database.
To date, we have published two manuscripts and submitted a third:
A project looking at the quality of information on robotic colorectal surgery using a machine learning algorithm called Web Scraping was recently accepted for publication in Computer Assisted Surgery (PMID 36905397). The second publication was aimed at developing and validating a prediction model for the cost of colon surgery. This was published in Frontiers in Surgery (PMID 36420401). The two submitted papers looked at the incidence of second primary tumors in patients that developed papillary thyroid cancer after the Chernobyl accident as this data has recently become publicly available for study.
In addition, we are currently working with machine learning algorithms to identify the quality of information on colon cancer that patients see when they use search engines such as google. The goal of this project is to make the medical community that cares for patients with colon cancer aware of the likely low and incomplete quality of information that they may see when they search the internet. Additionally, it will provide patients with specific resources that include quality information on diagnosis, work-up, surgical and non-surgical treatments. Dr. Jhang has recently agreed to start collaborative work in bariatrics with Dr. Taha.
Kathryn Verbanac, PhD.
Dr. Kathryn Verbanac, professor in East Carolina University’s Brody School of Medicine’s Department of Surgery, Division of Surgical Oncology, has been named Interim Director of ECU’s Brody School of Medicine Center for Health Disparities. She joined ECU after earning a PhD in Biochemistry at the University of Iowa, following her five years in biotechnology research. Verbanac’s focus on translational biomedical research has resulted in numerous peer-reviewed publications and over $5 million in extramural funding as PI/Co-PI, including a current award from the American Cancer Society. Her teaching responsibilities included medical and graduate courses via her adjunct appointment in microbiology and immunology. Verbanac has been consistently engaged as a research advisor and mentor for dozens of undergraduate and graduate students as well as medical residents, fellows and junior faculty.
Verbanac served as Assistant Vice Chancellor for research development and Director of the Office of Postdoctoral Affairs from 2014-2022. In that role, she fostered faculty development and facilitated interdisciplinary research bridging ECU campuses. Verbanac also co-authored and advised grant proposals for programs to increase the access of students and faculty from underrepresented groups in biomedical careers. Her research includes projects to identify and address barriers and disparities in breast cancer education, screening, treatment and outcome in eastern North Carolina. Verbanac has served on the Internal Advisory Board of the Center since 2018.
Shawn Moore, PhD.
Dr. Shawn Moore serves as Teaching Assistant Professor of Surgical Education for the Department of Surgery. His current role includes supporting residents’ curricular needs, supporting residents and attendings with assessment requirement from the ABS, and research development that will advance the education outcomes of the department and of the residency program. Dr. Moore’s research interests include understanding and enhancing how teaching and learning takes place in various surgical environments, the efficacy and transferability of mid-level fidelity surgical simulators compared to real world operations, and the use of assessment metrics as performance indicators that informs custom study plans. Dr. Moore received his Bachelor of Science degree in Biology, a Master of Science in Cell Biology/Immunology, and a Doctorate in Education, all from East Carolina University.
Education for the Department of Surgery. His current role includes supporting residents’ curricular needs, supporting residents and attendings with assessment requirement from the ABS, and research development that will advance the education outcomes of the department and of the residency program. Dr. Moore’s research interests include understanding and enhancing how teaching and learning takes place in various surgical environments, the efficacy and transferability of mid-level fidelity surgical simulators compared to real world operations, and the use of assessment metrics as performance indicators that informs custom study plans. Dr. Moore received his Bachelor of Science degree in Biology, a Master of Science in Cell Biology/Immunology, and a Doctorate in Education, all from East Carolina University.
Jane Ellen Blackerby

Jane Ellen Blackerby, from New Bern, NC, graduated from East Carolina University in 2021 with a BS in Public Health and a concentration in Community Health. Jane Ellen completed her Master’s in Public Health with a concentration in Epidemiology at ECU in the 2023 summer. She joined our team this summer and took the role of Social Clinical Research Specialist and is excited to further her career and experience in Greenville, NC.
Two new ecuBIC Reports
ORIC and REDE IT staff have been working hard to create two new ecuBIC reports intended to aid with identifying individuals who have submitted a Project Specific Disclosure (PSD) for a sponsored project. We hope these reports will be helpful and we look forward to hearing your feedback.” Both reports are available here and include:
- COI-PSD by eTRACS Proposal Number
- This report lists all individuals who have submitted project-specific conflict of interest (COI) disclosures in COI Risk Manager for a particular sponsored project using the eTRACS proposal number as the search input. Report results are delayed by one calendar day. Any active EHRA, SHRA, or CSS employee may access this report.
- NOTE: The report does not reconcile records submitted in COI Risk Manager with those individuals listed on an eTRACS proposal. This will still need to be done manually.
- COI-Project Specific Disclosure by User ID
- This report lists all eTRACS proposal numbers for which the user executing the report has submitted project-specific COI disclosures in COI Risk Manager. Report results are delayed by one calendar day. Any user with ecuBIC access may access this report, but only users who have submitted a COI-PSD will receive results.
Please direct questions or comments to oric@ecu.edu
Faculty can Receive Support to Publish Open Access Through: Open Access Phishing Support Fund
The Open Access Publishing Support Fund (OAPSF), sponsored by ECU Libraries, is available to help with article processing and open access charges for open access publishing. We welcome applications from current faculty, staff, graduate students, postdoctoral scholars or resident physicians.
For more information about the OAPSF and to apply, please visit: go.ecu.edu/openaccess.
For additional information and support for open access publishing, visit our Sustainable Scholarship website: https://sustainablescholarship.ecu.edu/.
QUESTIONS? Please contact us at scholarlycomm@ecu.edu with any questions.
Office of Clinical Research (ORC)
The ECU Clinical Trials Office (CTO) and the ECU Health Center for Research and Grants (CRG) have integrated to become the Office of Clinical Research (OCR). As such, there will be changes in the coming months related to clinical research study startup, operations, and finance. Please feel free to reach out to Cierra Buckman (buckmanc17@ecu.edu) if you have any questions. Below are a few immediate changes that have taken place:
- Ancillary Review – For studies that utilize health system services (lab, pathology, pharmacy, etc.), we will no longer have pre-ancillary protocol breakdown meetings or ancillary workgroup meetings. Aligning with ECU ancillary processes, ancillary reviewers will manage responses in epirate as it hits their queue. We highly encourage research teams to engage the ancillary departments for studies that might require more nuanced services. Cierra is working to compile both a rubric and directory of ancillary reviewers, so please be patient as the process evolves this summer.
- Data Requests – EMR data requests will no longer require the paper form to be filled out and submitted to crg.data@ecuhealth.org. This inbox is being disabled and we will be routing all data requests (inpatient and ambulatory) through this link. If you have questions about this process, please email Jason Buskirk, VP of Enterprise Data and Analytics at Jason.Buskirk@ecuhealth.org.
NOTE: If you have EPIC access, you should be able to log in with your EPIC credentials. If you do not have access to EPIC, you can call the Help Desk at 252-847-5111 and they can put in a data request for you, or help you with getting EPIC access if needed. We will notify everyone if additional login options become available for ECU-only affiliates in the future.
- eTracs Budget Changes for Contracts that route through the Office of Clinical Research
For studies that would route through the Office of Clinical Research (the integrated team that was previously Clinical Trials Office and Center for Research and Grants), we are making the following changes to budgets and eTracs applications:
-
- For studies where the total amount of the award is unknown, such as studies that are paid based on enrollments, we will no longer require an internal budget. The final sponsor budget will still need to be added to the application. On the budget screen, you will enter a $0 budget rather than estimating a budget.
-
- For studies where the total amount of the award is known, such as grants or studies that are contingent on milestones, you will add all the details of the budget to the budget screen and upload a budget justification within the budget tab. You will not need to do an internal budget for these studies either.
-
- For studies that will utilize ECU Health billable services, please upload a signed copy and excel copy of the final Services Review Form under the “Pre-Review Route & Attachments” tab. We will use this to generate work orders.
Note: for proposals routing through ORA, please continue to follow their office’s guidance.
- CRG Pricing Process Going forward, please send pricing requests to CRG.billing@ecuhealth.org and Teresa VanHeukelom (tvanheuk@ecuhealth.org) rather than Abner and the ancillary email address. The rest of the process will stay the same. If your study will involve the health system for services, procedures, and/or treatment, please email the above contacts while preparing your IRB application once you have your SRF drafted. Please also attach a copy of the study protocol using the following template email:
Subject: New Study Pricing Request [UMCIRB #]
Body of message:
Study Title: [Short title is fine]
UMC IRB #: [Should match ePirate]
PI: [Full name and Department]
Where will the study take place: [Outpatient, Inpatient, or Mix (for studies where patient may receive treatment in ECU Health Day Hospitals)]
If “Inpatient” or “Mix” – a protocol breakdown will be scheduled.
If “Inpatient” or “Mix” – please provide target MM/YY of SIV (if industry) or first enrollment (if not industry)
ECU Health Engagement: [Vendor for Labs / Imagining, Treatment (Hospital Pharmacy would be responsible for drug/device), or Other]
Please list any unusual tests / procedures in email. Please also consult the CPT code book on the CTO intranet when finalizing your SRF to ensure you are using a code that hospital has in their system.
Type of Study: [Industry sponsored, Federally Funded (medicare rates would apply), Cooperative Group, or Other]
- Compliance Reviews for Clinical Trials Changing Effective 6/28/23
All ECUP clinical trial reviews (new and ongoing studies) that were previously reviewed by the Office of Institutional Integrity will be transitioned to ECU Health Compliance starting July 1st. As of 6/28/23, any CTPLs OII receives will be forwarded to Carla McKeithan (Carla.McKeithan@ecuhealth.org). Moving forward, please remove OII staff names (Paula Brown and Lisa Heath) from your CTPL documents, and use the updated CTPL form (attached & available on the CTO intranet).
Questions email Cierra Buckman (buckmanc17@ecu.edu)
Mandatory Reseach Training for New Faculty in Clinical Departments
A new mandatory research training for new faculty hires in clinical departments provided by Cierra Buckman, MHS and Dr. Tumin, PhD has recently been announced. This will apply for faculty hires with 0.50 FTE or greater appointments July 1st forward, though we welcome any new faculty 0.50 FTE and below or faculty (full-time or part-time) that were brought on last fiscal year as well. This training will introduce important research topics and systems at the institution and orient faculty to resources available to support their research efforts. We will offer the training session once a quarter. All sessions will be held in-person. Below is the schedule for fiscal year 2024:
- July 27th from 9 am to 11 am
- October 26th from 9 am to 11 am
- February 8th from 9 am to 11 am
- April 25th from 9 am to 11 am
All new hires need to attend a session within their first year at the institution. To schedule, please email Cierra Buckman and Dr. Tumin the faculty’s name, a copy of their CV, and which session they will be attending at least one week prior to the session date. A reminder email will be sent out two weeks before each session.
Acute Care Surgery
In July, ECU Department of Surgery’s two Acute Care Surgery Fellows will be advancing their surgical careers! Thank you for your outstanding service!
 Lilly Bayouth, MD
Lilly Bayouth, MD
Medical School: University of Central Florida College of Medicine
Residency: East Carolina University/ECU Health Medical Center, Greenville, NC
What’s next? Lee Health Trauma in Ft Myer’s Florida
Greatest accomplishment while at ECU Health: “Becoming a Trauma Mama! I’ve learned how to successfully balance my commitment to my patients and still be present for my family.”
Surgical Research Areas of Interest: Pediatric Trauma Prevention
 Seth Welborn, MD
Seth Welborn, MD
Medical School: University of Pittsburgh School of Medicine
Residency: University of Louisville School of Medicine
What’s next? Kadlec Regional Medical Center in Richland, WA with former ECU fellow Dr. Mike Parmely.
Greatest accomplishment while at ECU Health: “I was most proud of being trusted to operate on a staff member. Everything went well!”
Surgical Research Areas of Interest: Quality Improvement Initiatives
CONGRATULATIONS to our 2023 Research Residents on their abstract submissions, presentations, education advancements and awards accomplished in their Research Year!

Greatest research accomplishment this year: POEM study completion.
Research areas/projects that I will continue: “I would like to continue foregut research with thoracic surgery and plastic surgery research.”

Greatest research accomplishment this year: “It’s tough to start and finish projects in only a year! That being said, the project I presented at the American Venous Forum in Feb 2023 is the best accomplishment this year. Although, I believe my Endologix paper will be exciting when we submit it to JVS. Outside of the actual projects, learning how to construct an IRB from start to finish in addition to becoming efficient at data collection/analyzing is an accomplishment I’m proud of.”
Research areas/projects that I will continue: Through ECU I will continue to be part of the Trauma, Glyburide and Papaverine projects. I’m also still working with Dr. Fleming and Dr. Yamaguchi on vascular surgery project ideas. Through UNC I will continue to work on my Endologix project.

Greatest research accomplishment this year: “Presenting our research at the American Association for Thoracic Surgery and the subsequent publication of our CABG AKI manuscript in JTCVS”
Research areas/projects that I will continue: “Several projects in both cardiac and thoracic surgery are ongoing and I will continue to work on them over the next couple years of residency. The project I am most excited about currently is a cost analysis of the non-narcotic protocol being used on our thoracic surgery service that we hope to present at a national meeting later this year.”

Greatest research accomplishment this year: “Winning the GME research week award.”
Research areas/projects that I will continue:
“I hope to continue my ongoing research in cancers of the colon, appendix and pancreas.”
Scholarships, Awards & Achievements:
June 2023: Congrats to Dr. Jesse O Mendes for completing his MBA from East Carolina University during his research year!
June 2023: Resident Awards Day:
Webex meeting recording: Surgical Grand Rounds 6.21.23-Resident Awards
Password: ZgFPYx*2
Recording link: https://ecu.webex.com/ecu/ldr.php?RCID=5890e1ac25c1f38cce17a6ec217b264b
Dept of Surgery Residents – GME Research Week award winners
Oral Presentations
Best Oral Presentation: Outcomes in Cardiac Valvular Surgery in Patients with Substance Use Disorder in a Rural Tertiary Medical Center
-
-
- Dr. Jacob Owen (General Surgery)
-
Clinical and Basic Science Research
Best Poster: Implementation of a Multimodal Pain Management Protocol Does Not Increase Hospitalization Cost After Thoracic
-
-
- Dr. Tia Sutton (General Surgery)
-
Honorable Mention Poster: Infectious Complications After Modified Purse-String Stomal Closure
-
-
- Dr. Scarlett Hao (General Surgery)
-
Brody Scholars:
Brooke Allen
 Brooke Allen is a second-year medical student at the Brody School of Medicine at East Carolina University. She graduated from Davidson College in May of 2020 with a Bachelor of Science in Biology and Hispanic Studies. After completing undergraduate, Brooke worked as a clinical research coordinator under Wendy Lane, MD at Mountain Diabetes and Endocrine Center in Asheville, NC. Her academic interests include surgical outcomes research with an emphasis on the causes of healthcare disparities.
Brooke Allen is a second-year medical student at the Brody School of Medicine at East Carolina University. She graduated from Davidson College in May of 2020 with a Bachelor of Science in Biology and Hispanic Studies. After completing undergraduate, Brooke worked as a clinical research coordinator under Wendy Lane, MD at Mountain Diabetes and Endocrine Center in Asheville, NC. Her academic interests include surgical outcomes research with an emphasis on the causes of healthcare disparities.
Amanda Landry
I am an MS2 at the Brody School of Medicine at ECU, currently involved in transplant  research with the ECU Department of Surgery.I graduated from UNCW with a BA in Psychology and Neuroscience, and then completed graduate school at UNC School of Medicine-Dept. of Allied Health Sciences with an MS in Clinical Rehabilitation & Mental Health Counseling. While at UNC, I worked in the department of transplant where I conducted pre and post-transplant psychological evaluations, and provided counseling to patients. I later worked as a clinical cognitive therapist specializing in traumatic brain injury rehabilitation for a non-profit organization in Raleigh, NC, and then later worked as a clinical trial project director/clinical therapist focusing on Rare and Orphan Diseases in children with VeraSci in Durham, NC. My academic interests include mitigating barriers impacting positive surgical outcomes, and addressing disparities unique to the southeastern U.S., which affect equitable access to quality care.
research with the ECU Department of Surgery.I graduated from UNCW with a BA in Psychology and Neuroscience, and then completed graduate school at UNC School of Medicine-Dept. of Allied Health Sciences with an MS in Clinical Rehabilitation & Mental Health Counseling. While at UNC, I worked in the department of transplant where I conducted pre and post-transplant psychological evaluations, and provided counseling to patients. I later worked as a clinical cognitive therapist specializing in traumatic brain injury rehabilitation for a non-profit organization in Raleigh, NC, and then later worked as a clinical trial project director/clinical therapist focusing on Rare and Orphan Diseases in children with VeraSci in Durham, NC. My academic interests include mitigating barriers impacting positive surgical outcomes, and addressing disparities unique to the southeastern U.S., which affect equitable access to quality care.
Brian Kang
 My name is Brian Kang. I was born in Seoul, South Korea and immigrated to the United States of America when I was 11 years old. Since then, I was born and raised in North Carolina. I graduated from UNC Chapel Hill with Physics and Music majors in 2014 and graduated from NC State University with a master’s degree in physiology in 2016. I am currently an M2 at ECU Brody SOM. I love watching and playing soccer and tennis.
My name is Brian Kang. I was born in Seoul, South Korea and immigrated to the United States of America when I was 11 years old. Since then, I was born and raised in North Carolina. I graduated from UNC Chapel Hill with Physics and Music majors in 2014 and graduated from NC State University with a master’s degree in physiology in 2016. I am currently an M2 at ECU Brody SOM. I love watching and playing soccer and tennis.
Brody Med Students:
Arvind Mallikarjunan – Transplantation
Arvind Mallikarjunan is a rising M2 at the Brody School of Medicine from Durham, NC. Arvind received his undergraduate degree from UNC-Chapel Hill in both Music and Exercise and Sport Science, and his Masters’ degree in Physiology from NC State. Previous to medical school, Arvind was a researcher at the Duke University Sickle Cell Comprehensive Care Center and is interested in using technology and machine learning models to improve patient care. Arvind is currently undecided in regard to his specialty and spends his free time playing saxophone, writing music, and hanging out with his pet tortoises.
from Durham, NC. Arvind received his undergraduate degree from UNC-Chapel Hill in both Music and Exercise and Sport Science, and his Masters’ degree in Physiology from NC State. Previous to medical school, Arvind was a researcher at the Duke University Sickle Cell Comprehensive Care Center and is interested in using technology and machine learning models to improve patient care. Arvind is currently undecided in regard to his specialty and spends his free time playing saxophone, writing music, and hanging out with his pet tortoises.
Kegan Cox – Trauma

My name is Kegan Cox and I am an M2 at Brody School of Medicine. I am originally from Wilmington, NC and obtained my B.S. in Biology with minors in Chemistry and Medical Anthropology at UNC Chapel hill. Prior to my matriculation to medical school, I worked as a clinical research coordinator for the Trauma/ ACS Department at CMC Main in Charlotte, NC. Here I cultivated a love for both research and surgery. I am thankful for the opportunity to continue pursuing research while in medical school!”
Campbell University, DO Students:
Rachel Grant
Rachel Grant is a second year medical student at Campbell University School of Osteopathic Medicine. She graduated from the University of Georgia with a Bachelors of Science in biology and minor in chemistry. She played two years of college soccer for Lincoln Memorial University and rowed for the University of Georgia Rowing Club. Before attending medical school, she worked for two years as an EMT in Atlanta at Grady EMS. She is interested in becoming a trauma surgeon.
University of Georgia with a Bachelors of Science in biology and minor in chemistry. She played two years of college soccer for Lincoln Memorial University and rowed for the University of Georgia Rowing Club. Before attending medical school, she worked for two years as an EMT in Atlanta at Grady EMS. She is interested in becoming a trauma surgeon.
David Cole Mueller
 Cole Mueller is a second-year medical student at Campbell University and is working with our Transplant and Surgical Oncology teams to further his medical career. While hailing from Pittsburgh, PA, he calls Matthews, NC home and desires to spend his life working in a similarly small town. In his free time Cole and his dog spend their time providing pet therapy, looking for swimming holes, and staying up late to watch the Penguins play hockey or reading fiction.
Cole Mueller is a second-year medical student at Campbell University and is working with our Transplant and Surgical Oncology teams to further his medical career. While hailing from Pittsburgh, PA, he calls Matthews, NC home and desires to spend his life working in a similarly small town. In his free time Cole and his dog spend their time providing pet therapy, looking for swimming holes, and staying up late to watch the Penguins play hockey or reading fiction.
MPH Students:
Efosa Iyore – MPH
Hi, my name is Efosa Iyore, and I am thrilled to be an MPH student intern at the ECU Division of Surgical Research. I am currently pursuing my Master of Public Health Degree at ECU Brody School of Medicine with a concentration in Health Policy, Administration, and Leadership (HPAL). I am excited to gain practical experience in the field of surgical research and its intersection with public health, contributing to the division’s mission of improving patient care. I am committed to learning as much as possible during my applied practicum experience and helping the team in any way I can. Outside of school and work, I enjoy reading, cooking, exercising, and playing soccer. After completing my program, I plan to continue my education in Medical School. I am grateful for this position and look forward to a fulfilling and rewarding internship experience.
I am currently pursuing my Master of Public Health Degree at ECU Brody School of Medicine with a concentration in Health Policy, Administration, and Leadership (HPAL). I am excited to gain practical experience in the field of surgical research and its intersection with public health, contributing to the division’s mission of improving patient care. I am committed to learning as much as possible during my applied practicum experience and helping the team in any way I can. Outside of school and work, I enjoy reading, cooking, exercising, and playing soccer. After completing my program, I plan to continue my education in Medical School. I am grateful for this position and look forward to a fulfilling and rewarding internship experience.
Emilyn Free – MPH

My name is Emilyn Free and I am currently in the MPH program here at East Carolina University with a concentration in Epidemiology .I am from Salisbury, NC but received my undergraduate degree in Medical Studies from Lenoir-Rhyne University. In my free time I enjoy hiking and listening to music. I look forward to spending the summer in this department.
Medical Students interested in surgical research
The mission of the Division of Surgical Research is to improve patient care, provide education in the pursuit of clinical and basic science investigations and health services research, and offer support to faculty, residents and students in the conduct, analysis and reporting of scientific inquiry.
If you are interested in getting involved in surgical research, contact surgeryresearch@ecu.edu to provide a brief orientation and review of your research interest/s.
Surgical Research Clinical Trials
Currently Enrolling Studies
| Area of Study | Title | Type | Accrual | PI | Contact Info |
|---|---|---|---|---|---|
| Surg Onc | Transportation Barriers to Care in Rural Cancer Patients | Observational | Dr. Drew Honaker | Study Coordinator Kelly Martin martinke21@ecu.edu 744-5723 |
|
| Surg Onc/Pancreas | Trans Intra-arterial Gemcitabine vs. Continuation of IV Gemcitabine plus Nab-Paclitaxel and Radiotherapy for Unresectable Locally Advanced Pancreatic Cancer | Phase II Trial | 11/12 | Dr. Emmanuel Zervos Dr. Andrew Ju | Study Coordinator Denise Brigham brighamd@ecu.edu 744-4924 |
| Surg Onc/Pancreas | Comparing the Clinical Impact of Pancreatic Cyst Surveillance Programs | Interventional | 3/10 | Dr. Emmanuel Zervos Dr. Andrew Ju | Study Coordinator Leslie Corbett corbettl@ecu.edu 744-0456 |
| Surg Onc/Soft Tissue | A Phase III Randomized Trial Comparing Adjuvant MK-3475 (Pembrolizumab) to Standard of Care Observation in Completely Resected Merkel Cell Carcinoma (NCT) | Phase III Trial | 3/2 | Dr. Nasreen Vohra | Study Coordinator Leslie Corbett corbettl@ecu.edu 744-0456 |
| Surg Onc/Soft Tissue | A Phase II Randomized Study of Adjuvant Versus NeoAdjuvant MK-3475 (Pembrolizumab) for Clinically Detectable Stage III-IV High Risk Melanoma | Phase II Trial | Closed to enrollment 5 in follow-up | Dr. Nasreen Vohra | Study Coordinator Leslie Corbett corbettl@ecu.edu 744-0456 |
| Transplant | TRULO - TruGraf Long-term clinical Outcomes | Observational | Closed to enrollment 81 in follow-up | Dr. David Leeser | Study Coordinator Peyton Garris garrisp21@ecu.edu 744-0114 |
| Transplant | ProActive - The PROspera Kidney Transplant ACTIVE Rejection Assessment Registry | Observational | Closed to enrollment 70 in follow-up | Dr. David Leeser | Study Coordinator Peyton Garris garrisp21@ecu.edu 744-0114 |
| Transplant | APOLLO - APOL1 Long-term Kidney Transplantation Outcomes Network | Observational | Closed to enrollment 29 enrolled | Dr. David Leeser | Study Coordinator Peyton Garris garrisp21@ecu.edu 744-5363 |
(January 2023 – June 2023)
- Anastasios T Mitsakos, Eftechios Xanthoudakis, William Irish, Walter C Robey 3rd, Rebecca M Gilbird, Jessica Cringan, Carl E Haisch. The Resource Costs of Maintaining Learner Utilization of Simulation Center During the COVID-19 Am Surg. 2023 May. doi: 10.1177/00031348211058637
- Fallon Ngo, Richard D Urman, Wayne English, Shanu Kothari, Eric DeMaria, Anupama Wadhwa. An analysis of enhanced recovery pathways for bariatric surgery-preoperative fasting, carbohydrate loading, and aspiration risk: a position statement from the International Society for the Perioperative Care of Patients with Obesity. Surg Obes Relat Dis. 2023 doi:10.1016/j.soard.2022.12.030
- Anastasios T Mitsakos, William Irish, Eric J DeMaria, Walter J Pories, Maria S Body mass index and risk of mortality in patients undergoing bariatric surgery. Surg Endosc. 2020 February. doi: 10.1007/s00464-022-09651-7
- Matthew J Martin, Karen J Brasel, Carlos V R Brown, Jennifer L Hartwell, Marc de Moya, Kenji Inaba, Eric J Ley, Ernest E Moore, Kimberely A Peck, Anne G Rizzo, Nelson G Rosen, Jordan A Weinberg, Raul Coimbra, Marie Crandall, Kaushik Mukherjee, Romeo Ignacio, Shannon Longshore, Katherine T Flynn- O’Brien, Grace Ng, Leigh Selesner, Mubeen Jafri. Pediatric Emergency Resuscitative Thoracotomy: A Western Trauma Association, Pediatric Trauma Association for the Surgery of Trauma Collaborative Critical Decisions Algorithm. J Trauma Acute Care Surg. 2023 doi: 10.1097/TA.0000000000004055
- Veronica Urbik, Zahra Mohseni, Dmitry Tumin, Shannon Longshore. In-Person school attendance and adolescent exposure to injury-related risk behaviors during the COVID-19 pandemic in the United Prev Med. 2023 June. doi: 10.1016/j.ypmed.2023.107502
- Anas Taha, Stephanie Taha-Mehlitz, Niklas Ortlieb, Vincent Ochs, Michael Drew Honaker, Robert Rosenberg, Johan F Lock, Martin Bolli, Phillippe C Cattin. Machine learning in pancreas surgery, what is new? Literature review. Front Surg. 2023 June. doi: 10.3389/fsurg.2023.1142585
- Brandon Peine, Kieran J Ved, Tyler Fleming, Ying Sun, Michael D Honaker. Syphilitic proctitis presenting as locally advanced rectal cancer: A case report. Int J Surg Case Rep. 2023 June. doi: 10.1016/j.ijscr.2023.108358
- Michael D Honaker, William Irish, Alexander A Parikh, Rebecca A Snyder. ASO Author Reflections: Rural- Urban Disparities in Colon Cancer Care: Trying to Close the Gap. Ann Surg Onc. 2023 doi: 10.1245/s10434-023-13381-y
- Michael D Honaker, William Irish, Alexander A Parikh, Rebecca A Snyder. ASO Visual Abstract: Association of Rural Residence and Receipt of Guideline Concordant Care for Locoregional Colon Cancer. Ann Surg Onc. 2023 June. doi: 10.1245/s10434-023-13403
- Michael D Honaker, William Irish, Alexander A Parikh, Rebecca A Snyder. Association of Rural Residence and Receipt of Guideline- Concordant Care for Locoregional Colon Cancer. Ann Surg Onc. 2023 June. doi: 1245/s10434-023-13340-7
- Scarlett Hao, David Meyer, Charles Klose, William Irish, Michael D Honaker. Association of distance traveled on receipt of surgery in patients with locally advanced rectal cancer. Int J Colorectal 2023 Jan. doi: 10.1007/s00384-022-04300-w
- Joshua R Aldridge, Seth A Quinn, Brandon S Peine, William D Irish, Eric A Toschlog. A Statewide Analysis of Predictors of Trauma Center Transfer. The Burden of Non-Clinical Factors. Am Surg. 2023 May. doi: 1177/00031348231173938
- Seth A Quinn, Stephen E Gregg, Nicole Garcia, Yuanyuan Fu, William Irish, Eric A Toschlog. Patterns of Platelet Mapping Thromboelastography Abnormalities in Trauma. Am Surg. 2023 March. doi: 1177/00031348231161668
- Christina M. Regelsberger-Alvarez, Christopher Pfeifer. Richter Hernia. 2023 Bookshelf ID: NBK537227
- Scott Friedberg, David Choi, Thomas Hunold, Natalie K Choi, Nicole M Garcia, Emma Picker, Nathaniel A Cohen, Russel D Cohen, Sushila R Dalal, Joel Pekow, Atsushi Sakuraba, Noa Krugliak, Cleveland, David T Rubin. Upadacitinib Is Effective and Safe in Both Ulcerative Colitis and Crohn’s Disease: Prospective Real- World Experience. Clin Gastroenterol Hepatol. 2023 Jul. doi: 10.1016/j.cgh.2023.03.001
- Brandon Peine, Yuanyuan Fu, SaeRam Oh, Seth Quinn, J Preston Bethea, O Jesse Mendes, Linda Kindell, William Irish, Shahab A Akhter. Impact of Timing of Urgent Coronary Artery Bypass Grafting Following Coronary Angiography on Acute Kidney Injury. J Thorac Cardiovasc Surg. 2023 June. doi: 1016/j.jtcvs.2023.05.042
- Joshua E McGee, Kate S Early, Anna C Huff, Marie C Clunan, Nicole R Hursey, Briceida Osborne, Colleen Bucher, Charles Tanner, Savannah B Brewer, Patricia M Brophy, Angela Clark, Walter J Pories, Laura E Matarese, Joseph A Houmard, David Collier, Linda E May, Joseph M McClung, Conrad P Earnest, Damon L Swift. Effects of weight loss and weight loss maintenance on cardiac autonomic function in obesity: a randomized controlled trial. Appl Physiol Nutri Metab. 2023 May. doi: 10.1139/apnm-2023-0025
- A M Ali, E J DeMaria, Walter J Pories. Comment on: The role of preoperative toxicology screening in patients undergoing bariatric surgery. Surg Obes Relat Dis. 2023 March. doi: 10.1016/j.soard.2022.12.009
- Damon L Swift, Joshua E McGee, Emily E Grammer, Anna C Huff, Marie C Clunan, Nicole Hursey, Taylor T Brown, Briceida G Osborne, Joseph A Houmard, Robert A Carels, Walter J Pories, Laura E Matarese. The effect of exercise training level on arterial stiffness after clinically significant weight loss. Clin Obes. 2023 February. doi: 10.1111/cob.12584
- Kylie N Nowicki, Walter J Pories. Bacteria with potential: Improving outcomes through probiotic use following Roux-en-Y gastric bypass. Clin Obese. 2023 February. doi: 10.1111/cob.12552
- Helen M Johnson, Anas Mohamed, Muhammed M Hassan, Joseph Geradts, Lauren Geisel, Nasreen A Vohra, Jan H Wong. Race-Related Differences in the Clinical Presentation and Histopathologic Features of Phyllodes Tumor. Am Surg. 2023 March. doi: 10.1177/00031348211029841
We could all use a little good news, so share yours with the Surgical Research Team!
We are looking for you to share any grants, abstracts, manuscripts and/or research related activity.
Send your good news (and photos) to our division email (surgeryresearch@ecu.edu) to be included in the next SURE Monthly Insider or Biannual Insight Newsletter.