SURGERY RESEARCH INSIGHT
Spring 2022
Surgical Health Care Disparities Research
Surgical health care disparities remain a significant public health concern in the United States. Mitigating surgical disparities is a priority of the American College of Surgeons, the National Institute of Health, and the US Department of Health and Human Services Healthy People Initiative. Numerous studies have demonstrated that access to surgical care is influenced by multiple factors but has historically been framed within the context of race/ethnicity. A systematic review of the literature on disparities in surgical access, defined 223 disparity measures within the categories of race, income, insurance, education, and geography that are associated with surgical disparities. Optimizing access is considered the key to quality surgical care.
Beyond the obligation to provide equitable care that does not vary in quality is the need to provide safe, timely, effective, and patient centered care and to assure that the care delivered is efficient. Surgical disparities result in substantial economic cost in terms of medical care for later presentation of disease, loss economic productivity, and years of life lost. A report on the economic burden of health inequalities sites that the elimination of health disparities for minorities would have reduced direct medical care expenditures by $229.4 billion for the years 2003-2006, some percentage of which could be attributable to surgical disparities.
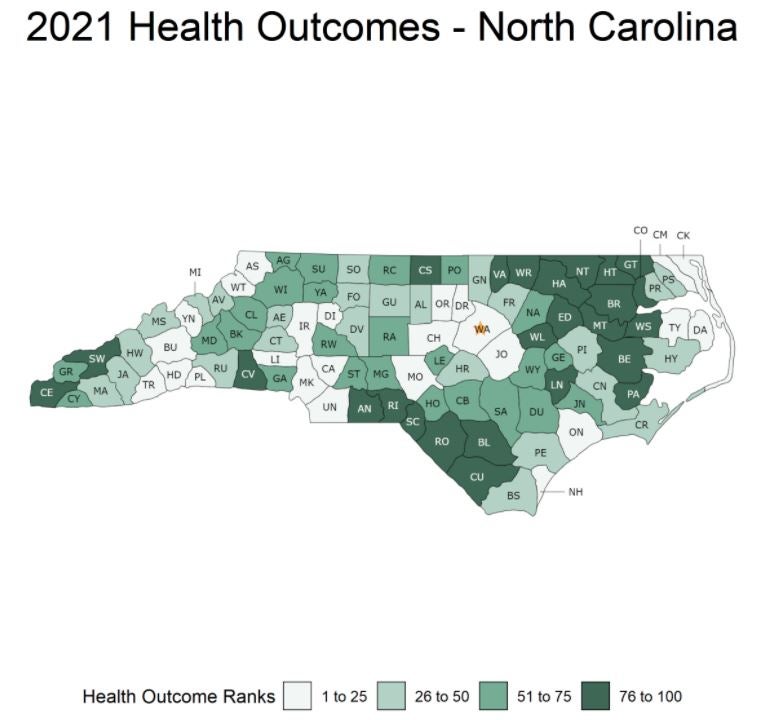
Eastern North Carolina is a large subregion of North Carolina that is medically served by the Brody School of Medicine. The population is poor, older, and less well educated than the rest of the US. The proportion of African Americans is generally above 30% in most counties. These are factors known to be associated with poorer health outcomes. Cancer disproportionately affects the region. Cancer (all site) mortality is 11% greater and breast cancer mortality is 19% greater than in the rest of North Carolina. The reasons for these poorer outcomes are assuredly multifactorial but gaps in care within certain segments of the population contribute to these disparate outcomes. Consistent with the Mission of the Brody School of Medicine which in part is “To improve the health status of eastern North Carolina’s citizens”, identifying and understanding surgical health care disparities with the overall goal of designing interventions to reduce these disparities is a major research focus of the Division of Surgical Research, East Carolina University Department of Surgery.
To date, most investigations of surgical disparities have focused on the components of the complex system and how they interact linearly to explain an observed disparate outcome. The assumptions in these studies, often unstated, may not hold for the health system. The determinants of surgical access disparities are broad, multifactorial, and inter-related. The delivery of optimal surgical care is the results of a network of multiple components broadly characterized as the health system (hospitals, clinics, rehabilitation centers, nursing homes), patients, and providers that interact on multiple levels and on different scales within a complex geographic, biologic, and social system. Understanding these inter-relationships is crucial to alleviating barriers to surgical access. Our research framework to advancing access to surgical care requires understanding complex inter-relationships between the patient, the provider, the clinical encounter, and the health care system from diagnosis through treatment and beyond involves complex diagnostic analytics to gain insight into disparities in surgical access from which novel informed interventions to mitigate those disparities can be developed.
Ongoing surgical disparities research areas of interest:
Surgical Oncology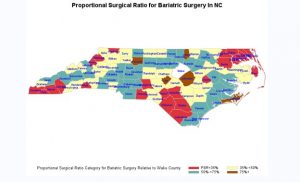
- Survey of Disparities and Barriers to Telehealth Use Among Cancer Patients
- Cancer Care Access for Rural Patients
- Understanding Disparities in Colorectal Cancer Outcomes in Eastern North Carolina
- Disparities in Distance and Time to Treatment for Colorectal Cancer
- Are there racial differences in rates of venous thromboembolism following major cancer surgery?
Trauma
General/Bariatric
-
- Proportional Surgical Ratio for Bariatric Surgery in NC
NC State University ASSIST Center Team Presents Biosensor Technology


On March 31, 2022, Kaila Peterson and Tanner Songkakul, post-doctoral students at NC State University visited with our team as part of our collaboration with the ASSIST Center. This visit included a presentation showcasing their health and environment tracker (HET) design and manufacturing, current timelines, and future collaboration projects. They also provided a demonstration of the technology and allowed our team to test these biosensors.
Prevalent use of wearable devices has recently increased significantly as they decrease the patient dependence on bulky medical equipment. These devices can be used in various areas such as remote health monitoring, early detection of diseases, post-surgery health monitoring, and physical performance monitoring. To meet this need, wearable electronics market has been dominated by various body-worn physiological sensors such as electrocardiography (ECG), electroencephalography (EEG), plethysmography (PPG), electromyography (EMG), pulse oximetry, skin temperature, and respiration.
However, the current wearables market is still in shortage of health monitoring devices for detection of other physiologically relevant biomarkers. The lack of such health monitoring devices limits the type and number of health conditions that can be monitored with the wearable devices we have access today. Upcoming projects in development may include exercise subjects and validating the clinical utility of the HET in a proof of concept study.


Upcoming Resident Research Workshop
We are excited to add depth to the surgical PGY4 research year!
This workshop provides basic instruction in all aspects of surgical research, including study start-up, developing the research question, developing the research plan, disseminating study results, and closing the study. These modules are designed to be interactive in nature with case studies and assignments throughout. The workshop will begin mid-July and last weekly through the end of August.
For residents entering their research year, participation in the workshop is mandatory. Upcoming research residents should check their email for a
pre-assessment survey. Please make sure to complete by May 31, 2022.
American Cancer Society Research Scholar Grant Awarded to
Dr. Nasreen Vohra

Congratulations to Dr. Nasreen Vohra for being awarded an American Cancer Society Research Scholar Grant entitled “Sentinel Node Immune Signatures & Outcomes in Triple Negative Breast Cancer”
The immune microenvironment within primary triple negative breast cancer (TNBC) has been heavily investigated, however there remains a gap in our understanding of the immune microenvironment within the regional lymph nodes – the secondary lymphoid organs where lymphocytes encounter tumor antigen.
Dr. Nasreen Vohra, surgical oncologist, with a team of collaborators will perform RNASeq analysis of tumor and corresponding SLN from 80 TNBC patients with a median follow up of >5 years. They will compare the DC and Th2 signatures between primary tumor and SLN as well as between sentinel nodes, supervised on recurrence and cancer-related death.
Research team:
Nasreen Vohra, MD, Principal Investigator Kathryn Verbanac, PhD, Co-Investigator William Irish, PhD, Co-Investigator Joseph Geradts, PhD, Co-Investigator I-Hsuan “Shannon” Tsai PhD, Co-Investigator
SAGES Foundation Barbara Berci Memorial Award 2022 Awarded to
Dr. Maria Altieri

Congratulations to Dr. Maria Altieri for being awarded the SAGES Foundation Barabara Berci Award.
This award is given in honor and memory of Barbara Berci, SAGES Executive Director from 1984 to 1998, in recognition of the passion, dedication, energy, and vision that she brought to the SAGES organization and its management. The award also recognizes her commitment to resolving social injustices and developing opportunities for young SAGES members.
The purpose of this award is to accelerate leadership growth and career development of young surgeons nationally and within SAGES.
The award supports attendance at a designated leadership course (such as the ACS Surgeons as Leaders course, SUS Leadership Agility Program, or other approved courses) to challenge thought processes and optimize leadership skills to effect change in the surgical world! She received the award at the SAGES Annual Meeting in March 2022.
Surgical Research Clinical Trials
Currently Enrolling Studies
| Area of Study | Title | Type | Accrual | PI | Contact Info |
|---|---|---|---|---|---|
| Surg Onc | Transportation Barriers to Care in Rural Cancer Patients | Observational | Dr. Drew Honaker | Study Coordinator Kelly Martin martinke21@ecu.edu 744-5723 |
|
| Surg Onc/Pancreas | Trans Intra-arterial Gemcitabine vs. Continuation of IV Gemcitabine plus Nab-Paclitaxel and Radiotherapy for Unresectable Locally Advanced Pancreatic Cancer | Phase II Trial | 11/12 | Dr. Emmanuel Zervos Dr. Andrew Ju | Study Coordinator Denise Brigham brighamd@ecu.edu 744-4924 |
| Surg Onc/Pancreas | Comparing the Clinical Impact of Pancreatic Cyst Surveillance Programs | Interventional | 3/10 | Dr. Emmanuel Zervos Dr. Andrew Ju | Study Coordinator Leslie Corbett corbettl@ecu.edu 744-0456 |
| Surg Onc/Soft Tissue | A Phase III Randomized Trial Comparing Adjuvant MK-3475 (Pembrolizumab) to Standard of Care Observation in Completely Resected Merkel Cell Carcinoma (NCT) | Phase III Trial | 3/2 | Dr. Nasreen Vohra | Study Coordinator Leslie Corbett corbettl@ecu.edu 744-0456 |
| Surg Onc/Soft Tissue | A Phase II Randomized Study of Adjuvant Versus NeoAdjuvant MK-3475 (Pembrolizumab) for Clinically Detectable Stage III-IV High Risk Melanoma | Phase II Trial | Closed to enrollment 5 in follow-up | Dr. Nasreen Vohra | Study Coordinator Leslie Corbett corbettl@ecu.edu 744-0456 |
| Transplant | TRULO - TruGraf Long-term clinical Outcomes | Observational | Closed to enrollment 81 in follow-up | Dr. David Leeser | Study Coordinator Peyton Garris garrisp21@ecu.edu 744-0114 |
| Transplant | ProActive - The PROspera Kidney Transplant ACTIVE Rejection Assessment Registry | Observational | Closed to enrollment 70 in follow-up | Dr. David Leeser | Study Coordinator Peyton Garris garrisp21@ecu.edu 744-0114 |
| Transplant | APOLLO - APOL1 Long-term Kidney Transplantation Outcomes Network | Observational | Closed to enrollment 29 enrolled | Dr. David Leeser | Study Coordinator Peyton Garris garrisp21@ecu.edu 744-5363 |
New NIH Salary Cap
This Notice provides information regarding the salary limitation for NIH grant and cooperative agreement awards and extramural research and development contract awards.
Since 1990, Congress has legislatively mandated a limitation on direct salary for individuals under NIH grant and cooperative agreement awards (referred to here as a grant). The mandate appears in the annual appropriation act that provides authority for NIH to incur obligations for a given Fiscal Year (FY). At this time, NIH has not received an FY 2022 appropriation and is operating under a Continuing Resolution, the “Continuing Appropriations Act, 2022” (Public Law 117-70), that applies the terms and conditions of the Consolidated Appropriations Act, 2021.
The Consolidated Appropriations Act, 2021, restricts the amount of direct salary to Executive Level II of the Federal Executive pay scale. The Office of Personnel Management released new salary levels for the Executive Pay Scale and effective January 2, 2022, the salary limitation for Executive Level II is $203,700.
For more information visit: https://grants.nih.gov/grants/guide/notice-files/NOT-OD-22-076.html
New Disclosure Requirements from the NIH
| Type of Activity | Biographical Sketch | Other Support | Annual Project Reports | Post-Award Information Terms & Condition |
||
|---|---|---|---|---|---|---|
| Professional preparation (e.g., educational degrees) | X | |||||
| Organizational Affiliations and Appointments | X | |||||
| Academic, professional, or institutional appointments, whether or not remuneration is received, and whether full-time, part-time, or voluntary. | X | |||||
| All projects currently under construction from whatever source, and all ongoing projects, irrespective of whether support is provided through the proposing organization, or directly to the individual, and regardless of whether or not they have monetary value (e.g., even if the support received is in-king such as office /laboratory space, equipment, supplies, or employees.) | X | X | X | |||
| Current or pending participation in, or applications to, programs sponsored by foreign governments, instrumentalities, or entities, including foreign government-sponsored talent recruitment programs. | X (Appropriate placement may be contract-dependent) | X (Appropriate placement may be contract-dependent) | ||||
| In-kind contributions not intended for use on the project/proposal being proposed. | X | X | X | |||
| Visiting Scholars in Labs funded by an external entity | X | X | ||||
| Students and postdoctoral researchers funded by an external entity | X | X | X | |||
| Consulting that falls outside of an individual's appointment; separate from institution's agreement | X | X | X | |||
| Travel supported/paid by an external entity to perform research activities with an associated time commitment. | X | X | X |
Welcome Safana!
Safana Abdullah Algutaini, currently a junior student at ECU, joins the Division of Surgical Research team through the Federal Work-Study Program. She was born in Yemen and has been living in the United States since 2019. Safana plans to pursue a career in Cardiology. She completed, with honors, an Associate Degree in Science from Wake Tech Community College. Currently, she is pursuing a Bachelor of Science Degree in Biology, minoring in Psychology at ECU. Previous research Safana has been involved in includes COVID-19 and Cerebellar Atrophy disease research at the Wake Tech Honors program. Also, she completed an internship with the antibiotic resistance department with bacteria. She continues to collaborate with the NC State Genetics Department where she is working with investigators about genetic deficits. Additionally, she has authored two published books in Arabic and English. Safana has a passionate interest and aspirations in scientific research. In addition, Safana owns a non-profit organization that supports female and Middle Eastern authors. Needless to say, we are thrilled she has joined our team!
CONGRATULATIONS to our Residents on their recent abstract submissions and outstanding presentations!
Academic Surgical Congress (ASC)
Title: Changes in colorectal cancer presentation during the COVID-19 pandemic
Authors: Tia Sutton, MD; Simone Boney, Esther Madugu, Scarlett Hao, MD; Anna Lisa Ciarrocca, Michael D Honaker, FACS, FASCRS
Presenter: Scarlett Hao, MD
American Pediatric Surgical Association (APSA)
Title: Shelter in Place and an Alarming Increase in Penetrating Trauma in Children In North Carolina
Author: Lauren Arthur, MD
American Society of Colon and Rectal Surgeons (ASCRS)
Title: The Effect on Distance Traveled on Time to First Treatment for Stage II/III Rectal Cancer
Authors: Popowicz, S Hao, RA Snyder, AA Parikh, W Irish, MD Honaker
Association for Surgical Education (ASE)
Title: The Impact of Delays in Interfaculty Transfer on Outcomes in Elderly Trauma Patients
Authors: Seth A. Quinn MD, Jacob D. Edwards MD, Peter Buccini BS, Michael Parmley MD, Kenji Leonard MD, William Irish PhD, and Eric Toschlog MD
International Hepato-Pancreato Biliary Association – IHPBA
Title: The Effect of Health Insurance on Racial Disparities in Patients with Isolated Colorectal Liver Metastases
Authors: Mitsakos, Hao, Irish, Parikh, Snyder
Resident Driven Wellness Project
Title: Give Us Some Space: Effects of a Dedicated Workspace on Surgical Residents
Authors: Seth A. Quinn, MD; Tyler Fleming, MD; Michelle Brownstein, MD
Society of American Gastrointestinal Endoscopic Surgeons (SAGES)
Title: Comparative Outcomes of Laparoscopic and Robotic Approaches to Gastrectomy
Authors: Caitlin Takahashi, DO1; Jamie Glasser, MS2; Cassandra Schuster2; Jamie Huston, MS3; Ravi Shridhar, MD, PhD4; Kenneth Meredith, MD5
Society of Surgical Oncology (SSO)
Poster Title: Effect of Distance Traveled on Receipt of Surgery in Patients with Stage II/III Rectal Cancer
Presenter: Scarlett B Hao, MD
Title: Leveraging the Electronic Health Record to Measure Social Determinants of Health Data in Patients with Gastrointestinal Cancer: A Feasibility and Acceptability Study
Authors: Scarlett B Hao, MD;1 Stephanie B Jilcott-Pitts, PhD;2 John Iasiello, BA;3 Christopher Mejia, BS;3 Ashley W Quinn, MD;1 Patrycja Popowicz, MD;1 William Irish, PhD;1,2 Anastasios Mitsakos, MD;1 Alexander A Parikh, MD, MPH, FACS;1 Rebecca A Snyder, MD, MPH, FACS1,2
The Society for Surgery of the Alimentary Tract (SSAT)
Title: Patient-Reported Social Determinants of Health Needs do not Correlate with Census Tract Measures of Socioeconomic Disadvantage in Patients with Gastrointestinal Cancers
Authors: Hao, Scarlett; Wercholuk, Ashley; Popowicz, Patrycja; Iasiello, John A.; Mejia, Christopher W.; Parikh, Alexander; Snyder, Rebecca A

Just in case you missed it: Surgical Grand Rounds 4.27.22 – Resident Research Presentations
Password: Surgery2022!
Karen Kennamer
Karen is a 2013 Magna Cum Laude graduate of East Carolina University in Nursing. She worked as a registered nurse in medical oncology for six years. In 2019 she was awarded the R. William McConnell, MD Medical Student Scholarship. She is a current third year medical student pursuing general surgery. Her previous research experience includes the areas of psychiatry and oncology. She has joined our department to assist in the study title, “Early outcomes associated with de novo LCPT vs IR-TAC in a predominantly African American kidney transplant cohort” and other studies in development in the division of transplantation and surgical immunology. Her hobbies include cooking and cats.
Upcoming Conferences
| Conference | Conference Dates | Location | |||
|---|---|---|---|---|---|
| Safe States | August 20, 2024 | Portland, OR | |||
| NC/SC - American College of Surgeons (ACS)- Annual Meeting | August 23, 2024 | Isle of Palms, SC | |||
| American Association for the Surgery of Trauma (AAST)(TACS) | September 11, 2024 | Las Vegas, NV | |||
| Society of Black Academic Surgeons (SBAS) | September 19, 2024 | Davis, CA | |||
| American Society of Plastic Surgeons (ASPS) | September 26, 2024 | San Diego, CA | |||
| American Academy of Pediatrics (AAP) | September 27, 2024 | Orlando, FL | |||
| CHEST Annual Meeting | October 6, 2024 | Boston, MA | |||
| Association of Women Surgeons (AWS) | October 18, 2024 | San Francisco, CA | |||
| American College of Surgeons (ACS) | October 19, 2024 | San Francisco, CA | |||
| Surgical Outcomes Club (SOC) | October 19, 2024 | San Francisco, CA | |||
| Patient Centered Outcomes Research Institute (PCORI) | October 22, 2024 | Washington, D.C. | |||
| Kidney Week (ASN) | October 23, 2024 | San Diego, CA | |||
| Society of Immunotherapy of Cancer (SITC) | November 6, 2024 | Houston, TX | |||
| ACS TQIP | November 12, 2024 | Denver, CO | |||
| Southern Surgical Association (SSA) | December 8, 2024 | Palm Beach, FL | |||
| National Research Conference for the Prevention of Firearm Related Harms | December 9, 2024 | Seattle, WA | |||
| San Antonio Breast Cancer Symposium | December, 10, 2024 | San Antonio, TX |
Publications
(January 2022-May 2022)
1: Slama EM, Johnson HM, Yu YR, Sumra H, Altieri MS. Paid parental leave for
surgeons in the United States. Am J Surg. 2022 Jan;223(1):218-220. doi:
10.1016/j.amjsurg.2021.08.016.
2: Johnson HM, Torres MB, Tatebe LC, Altieri MS; from the Publications Committee
of the Association of Women Surgeons. Every ounce counts: A call for
comprehensive support for breastfeeding surgeons by the Association of Women
Surgeons. Am J Surg. 2022 Jan 5:S0002-9610(21)00785-6. doi:
10.1016/j.amjsurg.2021.12.037.
3: Bevilacqua LA, Siena NM, Gardner CA, Tatarian T, Madani A, Altieri MS. Gender
disparities among leadership in academic surgical publishing over the past
decade. Am J Surg. 2022 Jan;223(1):47-52. doi: 10.1016/j.amjsurg.2021.07.038.
4: Ieong K, Brown A, Yang J, Zhang X, Altieri MS, Spaniolas K, Pryor AD. The
incidence of reintervention and reoperation following Heller myotomy across
multiple indications. Surg Endosc. 2022 Feb;36(2):1619-1626. doi:
10.1007/s00464-021-08357-6.
5: Aminian A, Vosburg RW, Altieri MS, Hinojosa MW, Khorgami Z; American Society
for Metabolic and Bariatric Surgery Clinical Issues Committee. The American
Society for Metabolic and Bariatric Surgery (ASMBS) updated position statement
on perioperative venous thromboembolism prophylaxis in bariatric surgery. Surg
Obes Relat Dis. 2022 Feb;18(2):165-174. doi: 10.1016/j.soard.2021.10.023.
6: Altieri MS, DeMaria E, Lensing C, Derecho J, Fallorina R, Mehrotra S, Pories
W, Irish WD. Retrospective comparative study of the effectiveness of bariatric
surgery on 3-year outcomes in the real-world clinical setting. Surg Obes Relat Dis.
2022 Feb;18(2):196-204. doi: 10.1016/j.soard.2021.11.013
7: DeMaria EJ, Kothari SN, Rogers AM. VTE prevention in bariatric surgery: from
where have we come, and how did we get here? Surg Obes Relat Dis. 2022
Feb;18(2):175-176. doi: 10.1016/j.soard.2021.10.022.
8: Edwards JD, Quinn SA, Burchette M, Irish W, Poulin N, Toschlog EA. Direct
Peritoneal Resuscitation in Trauma Patients Results in Similar Rates of Intra-
Abdominal Complications. Surg Infect (Larchmt). 2022 Mar;23(2):113-118. doi:
10.1089/sur.2021.262.
9: Mitsakos AT, Irish W, Parikh AA, Snyder RA. The association of health
insurance and race with treatment and survival in patients with metastatic
colorectal cancer. PLoS One. 2022 Feb 17;17(2):e0263818. doi:
10.1371/journal.pone.0263818.
10: Edwards JD, Quinn SA, Saylors S, McBride K, Scott S, Irish W, Garcia N,
Toschlog E. Where to Draw the Line for Intracranial Hypertension; Opening
Pressures and Mortality. Am Surg. 2022 Mar 11:31348221080438. doi:
10.1177/00031348221080438.
11: Altieri MS, DeMaria E, Lensing C, Derecho J, Fallorina R, Mehrotra S, Pories
W, Irish WD. Real-world retrospective analysis of outcomes in patients
undergoing bariatric surgery with class 1 obesity. Surg Obes Relat Dis. 2022 Jan
25:S1550-7289(22)00027-2. doi: 10.1016/j.soard.2022.01.011.
12: Roll GR, Cooper M, Verbesey J, Veale JL, Ronin M, Irish W, Waterman AD,
Flechner SM, Leeser DB. Risk aversion in the use of complex kidneys in paired
exchange programs: Opportunities for even more transplants? Am J Transplant.
2022 Feb 18. doi: 10.1111/ajt.17008.
13: Hao S, Snyder RA, Irish W, Parikh AA. Correction: Association of race and
health insurance in treatment disparities of colon cancer: A retrospective
analysis utilizing a national population database in the United States. PLoS
Med. 2022 Feb 23;19(2):e1003937. doi: 10.1371/journal.pmed.1003937. Erratum for:
PLoS Med. 2021 Oct 25;18(10):e1003842.
14: Quinn SA, Edwards JD, Buccini P, Parmley MK, Leonard K, Irish W, Toschlog EA.
The Impact of Delays in Interfaculty Transfer on Outcomes in Elderly Trauma
Patients. Am Surg. 2022 Mar 24:31348221082278. doi: 10.1177/00031348221082278.
15: Hao S, Mitsakos A, Irish W, Tuttle-Newhall JE, Parikh AA, Snyder RA.
Differences in receipt of multimodality therapy by race, insurance status, and
socioeconomic disadvantage in patients with resected pancreatic cancer. J Surg
Oncol. 2022 Mar 22. doi: 10.1002/jso.26859.
16: Edwards JD, Quinn SA, Burchette M, Irish W, Poulin N, Toschlog EA. Direct
Peritoneal Resuscitation in Trauma Patients Results in Similar Rates of Intra-
Abdominal Complications. Surg Infect (Larchmt). 2022 Mar;23(2):113-118. doi:
10.1089/sur.2021.262.
17: Mitsakos AT, Irish W, Parikh AA, Snyder RA. The association of health
insurance and race with treatment and survival in patients with metastatic
colorectal cancer. PLoS One. 2022 Feb 17;17(2):e0263818. doi:
10.1371/journal.pone.0263818.
18: Edwards JD, Quinn SA, Saylors S, McBride K, Scott S, Irish W, Garcia N,
Toschlog E. Where to Draw the Line for Intracranial Hypertension; Opening
Pressures and Mortality. Am Surg. 2022 Mar 11:31348221080438. doi:
10.1177/00031348221080438.
19: Roll GR, Cooper M, Verbesey J, Veale JL, Ronin M, Irish W, Waterman AD,
Flechner SM, Leeser DB. Risk aversion in the use of complex kidneys in paired
exchange programs: Opportunities for even more transplants? Am J Transplant.
2022 Feb 18. doi: 10.1111/ajt.17008.
20: Hao S, Snyder RA, Irish W, Parikh AA. Correction: Association of race and
health insurance in treatment disparities of colon cancer: A retrospective
analysis utilizing a national population database in the United States. PLoS
Med. 2022 Feb 23;19(2):e1003937. doi: 10.1371/journal.pmed.1003937. Erratum for:
PLoS Med. 2021 Oct 25;18(10):e1003842.
21: Quinn SA, Edwards JD, Buccini P, Parmley MK, Leonard K, Irish W, Toschlog EA.
The Impact of Delays in Interfaculty Transfer on Outcomes in Elderly Trauma
Patients. Am Surg. 2022 Mar 24:31348221082278. doi: 10.1177/00031348221082278.
22: Hao S, Mitsakos A, Irish W, Tuttle-Newhall JE, Parikh AA, Snyder RA.
Differences in receipt of multimodality therapy by race, insurance status, and
socioeconomic disadvantage in patients with resected pancreatic cancer. J Surg
Oncol. 2022 Mar 22. doi: 10.1002/jso.26859.
23: Mohamed A, Kousar A, Wong J, Vohra N, Muzaffar M, Geradts J. Pathobiologic
Stratification of Oncotype DX Recurrence Scores and Comparative Validation of 3
Surrogate Models. Arch Pathol Lab Med. 2022 Feb 4. doi:
10.5858/arpa.2021-0367-OA.
24: Hao S, Parikh AA, Snyder RA. Racial Disparities in the Management of
Locoregional Colorectal Cancer. Surg Oncol Clin N Am. 2022 Jan;31(1):65-79. doi:
10.1016/j.soc.2021.07.008.
25: Snyder RA. A Soft Spot. J Clin Oncol. 2022 Mar 17:JCO2200068. doi:
10.1200/JCO.22.00068.
26: Snyder RA, Ahmad S, Katz MHG. Pancreas cancer trials for early stage disease:
Surgeons leading therapeutic cooperative group trials. J Surg Oncol. 2022
Jan;125(1):75-83. doi: 10.1002/jso.26701.
27: Keller DS, Snyder RA, Talimini M, Pawlik TM, Crowell K, Puri R, Fong ZV,
Zaman JA. “How to” Course for Resident Reviewers: from the Resident and Fellow
Education Committee of the Society for Surgery of the Alimentary Tract (SSAT). J
Gastrointest Surg. 2022 Feb;26(2):466-468. doi: 10.1007/s11605-021-05202-y.
28: Josef AP, Garcia NM. Systemic Anticoagulation and Reversal. Surg Clin North
Am. 2022 Feb;102(1):53-63. doi: 10.1016/j.suc.2021.09.011. PMID: 34800389.
29: Bennett S, Wanless S, Harris MP, Newell MA, Searle K, Green JA, Daunt F.
Site-dependent regulation of breeding success: Evidence for the buffer effect in
the common guillemot, a colonially breeding seabird. J Anim Ecol. 2022 Feb 14.
doi: 10.1111/1365-2656.13674.
30: Popowicz P, Leonard K. Noninvasive Ventilation and Oxygenation Strategies.
Surg Clin North Am. 2022 Feb;102(1):149-157. doi: 10.1016/j.suc.2021.09.012.
PMID: 34800383; PMCID: PMC8598279.
31: Patel H, Tumin D, Greene E, Ledoux M, Longshore S. Lack of Health Insurance
Coverage and Emergency Medical Service Transport for Pediatric Trauma Patients.
J Surg Res. 2022 Mar 24;276:136-142. doi: 10.1016/j.jss.2022.02.010.
32: Sheikh SS, Romine MM, Locke JE. The “Broken rung” in transplantation surgery.
Am J Surg. 2022 Mar 14:S0002-9610(22)00137-4. doi:
10.1016/j.amjsurg.2022.02.057.
33: Chipman V, Cooper M, Thomas AG, Ronin M, Lee B, Flechner S, Leeser D, Segev
DL, Mandelbrot DA, Lunow-Luke T, Syed S, Hil G, Freise CE, Waterman AD, Roll GR.
Motivations and outcomes of compatible living donor-recipient pairs in paired
exchange. Am J Transplant. 2022 Jan;22(1):266-273. doi: 10.1111/ajt.16821.
34: Roll GR, Cooper M, Verbesey J, Veale JL, Ronin M, Irish W, Waterman AD,
Flechner SM, Leeser DB. Risk aversion in the use of complex kidneys in paired
exchange programs: Opportunities for even more transplants? Am J Transplant.
2022 Feb 18. doi: 10.1111/ajt.17008. Epub ahead of print. PMID: 35181991.
35: Lim SA, Hao SB, Boyd BA, Mitsakos A, Irish W, Burke AM, Parikh AA,
Snyder RA.Opportunity Costs of Surgical Resection and Perioperative Chemotherapy
for locoregional Pancreatic Adenocarcinoma. JCO Oncol Pract. 2022 Apr;18(4):302-309.
doi: 10.1200/OP.21.00311. Epub 2021 Oct 28. PMID: 34709961.
36: David G, Gunnarsson C, Laine L, Ryan M, Clancy S, Gunnarsson G, Moore K,Irish W.
The unintended consequences of Medicare’s wage index adjustment on device-intensive
hospital procedures. Am J Manag Care. 2022 Mar1;28(3):e96-e102. doi: 10.37765/ajmc.
2022.88842. PMID: 35404553.
37: Edwards JD, Quinn SA, Burchette M, Irish W, Poulin N, Toschlog EA. Direct Peritoneal
Resuscitation in Trauma Patients Results in Similar Rates of Intra-Abdominal Complications.
Surg Infect (Larchmt). 2022 Mar;23(2):113-118. doi:10.1089/sur.2021.262. Epub 2021 Nov 23.
PMID: 34813370.
38: Gourash WF, King WC, Shirley E, Hinerman A, Ebel F, Pomp A, Pories WJ, Courcoulas AP.
Five-year attrition, active enrollment, and predictors of level of participation in the Longitudinal
Assessment of Bariatric Surgery (LABS-2)study. Surg Obes Relat Dis. 2022 Mar;18(3):394-403.
doi:10.1016/j.soard.2021.11.023. Epub 2021 Nov 27. PMID: 35027321.
39: Altieri MS, Irish W, Pories WJ, DeMaria EJ. The US Prevalence of MetabolicSurgery in
Patients with Obesity and Type 2 Diabetes Has Not Increased Despite Recommendations
from the American Diabetes Association. Obes Surg. 2022Apr;32(4):1086-1092.
doi: 10.1007/s11695-021-05865-1. Epub 2022 Jan 15. PMID:35032312.
40: Garfinkle R, Petersen RP, DuCoin C, Altieri MS, Aggarwal R, Pryor A, Zevin B.Consensus
priority research questions in gastrointestinal and endoscopic surgery in the year 2020:
results of a SAGES Delphi study. Surg Endosc. 2022 Jan 14.doi: 10.1007/s00464-021
-08941-w. Epub ahead of print. PMID: 35028734.
41: Akram WM, Vohra N, Irish W, Zervos EE, Wong J. Racial Disparity in the Surgical
Management of Diverticular Disease. Am Surg. 2022 May;88(5):929-935.doi:
10.1177/00031348211058623. Epub 2021 Dec 29. PMID: 34964694.
42: Hao S, Reis HL, Quinn AW, Snyder RA, Parikh AA. Prehabilitation for Older
Adults Undergoing Liver Resection: Getting Patients and Surgeons Up to Speed.
JAm Med Dir Assoc. 2022 Apr;23(4):547-554. doi: 10.1016/j.jamda.2022.01.077.
Epub2022 Mar 2. PMID: 35247359.
43: Maynard L, Howorth P, Daniels J, Bunney KL, Snyder R, Jenike D, Barnhart T,
Spevak E, Fitzgerald P, Gezon Z. Conservation psychology strategies for collaborative
planning and impact evaluation. Zoo Biol. 2022 Apr 12. doi:10.1002/zoo.21692.
Epub ahead of print. PMID: 35412653.
44: Lim SA, Hao SB, Boyd BA, Mitsakos A, Irish W, Burke AM, Parikh AA, Snyder RA.
Opportunity Costs of Surgical Resection and Perioperative Chemotherapy for locoregional
Pancreatic Adenocarcinoma. JCO Oncol Pract. 2022 Apr;18(4):302-309.doi:
10.1200/OP.21.00311. Epub 2021 Oct 28. PMID: 34709961.
45: Mitsakos AT, Vohra NA, Fitzgerald TL, Buccini P, Parikh AA, Snyder RA, Zervos.
Improvement in Surgical Quality Following Pancreaticoduodenectomy With
Increasing Case Volume in a Rural Hospital. Am Surg. 2022 Apr;88(4):746-751.
doi: 10.1177/00031348211050808. Epub 2021 Nov 18. PMID: 34792413.
46: Quinn S, Akram W, Hao S, Honaker MD. Emergency Surgery for Diverticulitis:
Relationship of Outcomes to Patient Age and Surgical Procedure. J Am Med DirAssoc.
2022 Apr;23(4):616-622.e1. doi: 10.1016/j.jamda.2022.02.001. Epub 2022Mar 1.
PMID: 35245484.